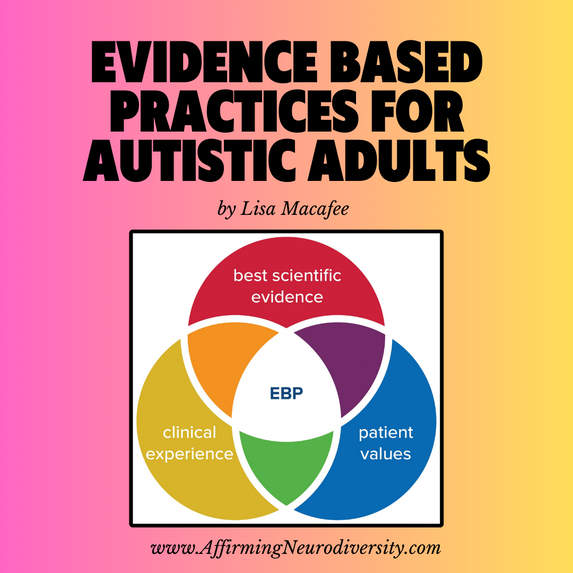
Evidence-Based Treatments For Autistic Adultsby Lisa Macafee Autistic gender diverse people may need different treatments than the typical population because their neurology is different from a neurotypical person’s. Queer autistic people experience disproportionate rates of mental and physical health troubles, including anxiety, depression, obsessive compulsive disorder, substance use disorder, increased smoking, early death, and other health conditions (Hall, et al., 2021). There is no established pharmacological treatment for autism (Aran et al., 2021) and traditional treatments can be difficult for autistic people due to challenges with sensory sensitivities, executive functioning, difficulty with theory of mind, identifying and managing emotions and feelings, and cognitive flexibility that many treatments rely on (Spain et al., 2020). Treatments such as group therapy, for example, may be especially unhelpful for autistic adults due to the pressures of social anxiety and personalized intervention plans are often needed (Helverschou et al., 2019). Evidence Based Treatment for Autistic Adults General Recommendations Autistic people face complex challenges when accessing health care, but there are some practical and simple strategies that providers can implement to make their practices more accessible. Doherty et al. (2022) state that challenges most common for autistic people are stressors involved in communication such as making appointments on the phone, being misunderstood or not listened to, not being able to follow along with what the providers is saying, sensory challenges in waiting rooms and offices, and lack of predictability for cancellations or wait times. Adjustments for autistic people can be implemented by providers understanding how autism impacts people and offering simple changes such as multiple modalities for scheduling appointments instead of requiring a phone call (Doherty et al., 2022). Mayor (2021) found that simple strategies adopted by health care providers can make significant differences in autistic people’s anxiety levels when seeking treatment. Phrasing questions in clear and concise language that cannot be misinterpreted, offering a quiet waiting space for appointments, seeing appointments on time, minimizing cancellations, and exhibiting patience, calm, and respect for clients makes seeking services much less anxiety-producing for autistic people (Mayor, 2021). Some of the best evidence based practices for autistic people can be learning about how autistic people function and finding basic techniques to reduce stress and maximize wellbeing. Ghanouni & Quirke (2023) found coping strategies that can be most effective for autistic people are engaging in their special interests, recreational and leisure activities, taking regular breaks for sensory and emotional regulation, regular socialization, and having supportive relationships. They state two generalized strategies useful for autistic people are problem-focused coping and emotion-focused coping where the individual focuses on mitigating negative emotions and attribute meaning to stressful situations. Especially noted as helpful for autistic adults were technology supports such as phone alarms and checklist apps that allow tracking of required daily tasks, but also technology used for social connection and networking. Technology supports help autistic people address needs without triggering social anxiety and timed social responses that can cause so much stress. Learning how autism affects individuals so they can understand and better moderate their challenges, understand their own strengths and weaknesses, learn more about other autistic people, and how the individual’s challenges are common or unique are beneficial to autistic overall wellbeing (Ghanouni & Quirke, 2023). Some simple strategies recommended by autistic AFAB people are to take time for oneself to prevent burnout, creating supportive routines and structure, and un-learning the tendency to mask all autistic behaviors as this often leads to increased stressors, and for some, loss of sense of self (Miner, et. all, 2019). Maladaptive coping strategies such as avoidance, self-blame, and masking should be avoided as they can lead to autistic burnout, a focus of intervention should be on leaning into healthy coping strategies and de-focusing unhealthy coping strategies (Ghanouni & Quirke, 2023). While autism is a marked by challenges in social function, that does not mean that socialization is not important for autistic people. Social inclusion, supportive social relationships, and feeling belonging can be helpful to increase resilience among autistic individuals (Ghanouni & Quirke, 2023). According to Djela (2021), one large impact to increase social inclusion, belonging, and increased social support for autistic people is finding productive employment. They state 77% of autistic adults are unemployed but want to work and only 16% work full-time. Autistic people are often undervalued and discriminated against in the workforce due to stigma and fear and having atypical behavioral or social responses, but often have underappreciated skills of work ethic, methodical approach to tasks, reliability, innovative thinking, and in-depth interest in topics (Djela, 2021). Autistic people can be productive employees that are true assets to their workplace with a few basic accommodations. Accommodations in the workplace such as not requiring social masking where the autistic person tries to appear typical, allowing noise cancelling earbuds, being able to take sensory breaks, and other steps can help autistic adults thrive at work and allow for more social engagement (Djela, 2021). Social engagement for autistic people can be just as important to mental health as for neurotypical people, there are simple challenges to be worked through for autistic people to do so. Cognitive Behavioral Therapy Adapted cognitive behavioral therapy (CBT) has been found to be especially effective for autistic adults. Autistic people using CBT therapies were found to have significant improvements in depression, anxiety, stress, social anxiety, fear, avoidance, and restricted and repetitive behaviors, and increase social motivation, and overall mental health (Bemmer et al., 2021). CBT is a goal-based form of talking therapy based on understanding the relationships between thoughts, feelings, and actions, identifying unhealthy thought patterns and developing effective coping strategies to stop harmful thought cycles, and trying to break patterns of thought that contribute to negative psychological states (Spain et al., 2020). Spain et al. (2020) state that CBT can be particularly helpful for autistic people, especially those with anxiety or obsessive-compulsive disorder (OCD) due to the formulaic structure of CBT, structured discussions that focus on practical details, collaboratively defined goals, and focus on implementing pragmatic strategies. Modified CBT has been one of the most helpful treatment options for up to 36% of autistic adults with substance use disorder, which is more common among social autistics without intellectual disability (Helverschou et al., 2019). For CBT to be effective for autistic people, there are accommodations that can be used to optimal use. To be most effective with literal minded autistic clients, practitioners can change session length to include enough time to discuss issues thoroughly and concretely, include more preparation and practical skill building, use repetition of tasks to create more comfortable routines that include special interests, and including other people in the client’s life such as family or teachers (Spain et al., 2020). These simple changes allow more comfort and practicality for autistic clients to implement CBT in their lives. Clinicians should also note that autistic clients may be more demanding and benefit from increased structure, more directive strategy implementation, high individualization of treatment, practical life support in areas of housing, life skills, and employment, and increased length and number of sessions compared to neurotypical clients (Helverschou et al., 2019). Exercise Simple remedies such as exercise can be helpful for autistic people and is associated in the general population with not only improved physical health but higher self-esteem, attention, self-efficacy, and reduced behavioral and emotional regulation problems (Tse, 2020). The ability to engage in physical tasks such as walking and exercise are associated with aging well and less health complications in autistic adults (Hwang et al., 2021). Tse (2020) states that for children with autism, exercise improved mood, emotional expression, emotional regulation, social functioning, and self-awareness, and decreased internal, and external behavioral problems such as stereotyped behaviors. These benefits may be due to serotonin, norepinephrine, and dopamine released by exercise that are associated with inhibition of behavior (Tse, 2020). While exercise is recommended as a healthy habit for all people, this can be especially important for mind-body integration and moderation of emotion in autism. Medication Treatments Due to differences in neurocognitive function among people with autism, medications often work differently for autistic people as compared to neurotypical people. Deb et al. (2021) state there is no evidence that older generation tricyclic antidepressant medications improve negative symptoms for autistic people and the risks of side effects and overdose make tricyclic antidepressants a poor choice for autistic people. They continue to state that research is lacking on anti-anxiety medications and newer antidepressants in the SSRI and serotonin-noradrenaline reuptake inhibitors group and only citalopram and buspirone have shown marginal benefit for autistic people, benzodiazepines and beta-blockers both have serious side effects and are not recommended for long term use. Overall, no significant benefits are seen for autistic people taking anti-depressants or anti-anxiety medications compared to placebo groups, which makes treatment for autistic adults difficult for modern medicine (Deb et al., 2021). Having no default medication recommendations for autistic people can be challenging to the modern medical system and requires more thoughtful consideration in treatment plans. Alternative Treatments With mainstream prescriptions found ineffective for treating autistic people with anxiety or depression or behavior and communication challenges, alternative treatments have been explored and found to be beneficial. Markopoulos et al. (2022) found that psychedelics such as lysergic acid diethylamide (LSD), psilocybin, and dimethyltryptamine (DMT), along with methylenedioxymethamphetamine (MDMA) have demonstrated ability to reduce social anxiety, increase pro-social behaviors, and increase empathy in autistic adults. For example, psylocibin has been found to increase openness and extraversion in people with treatment resistant depression up to three months after two sessions of therapy treatment. They continue to state LSD has been found to increase desire to be with other people, emotional empathy, sociability, trust, closeness, and blood levels of oxytocin. From the same study, LSD and psylocibin both reduce anxiety and depression symptoms and two therapy sessions of LSD allowed positive effects to last up to one year. Current research cannot say definitively if the use of psychedelics could be uniformly beneficial for autistic people due to the variety of symptomology and challenges autistic people experience and the possibility that the dysregulating effects of psychedelics would outweigh the prosocial benefits (Markopoulos et al., 2022). Cannabis has also shown positive outcomes to support autistic adults in escaping rigid maladaptive patterns of thought. Cannabis is associated with decreased hostile feelings and increased interpersonal communication ability (Aran et al., 2021). Aran et al. (2021) states that while THC can be associated with increased anxiety and psychosis and decreased motivation and cognitive decline, CBD seems to have antipsychotic, antiepileptic, and neuroprotective factors. They continue to say that cannabinoid treatment seems to improve social function and improve core challenges for 49% of autistic people compared to 21% who took a placebo. More research in alternative treatments would be beneficial as there are promising treatment options here. Applied Behavioral Analysis Applied behavioral analysis (ABA) is one of the more controversial treatments for autism. ABA consisting of analyzing behavior for antecedent, behaviors, and consequences, and using rewards and punishments to shape behaviors, and for many people in the United States it is the only treatment that insurance will pay for (Kirkham, 2017). While it has been found in research to be an effective treatment for some of the more challenging behaviors in autistic children, it is important to ask what criteria is being used to qualify studies as successful, children acting more typical or children learning strategies to live more full and happy lives (Tse, 2020). ABA has also been found to have caused complex PTSD in individuals who received classical ABA that utilize discrete trials, physical aversives, and repetition to replicate typical behavior from children at the cost of their own authentic behaviors, personality, judgment, and comfort (Kirkham, 2017). ABA done well with individualized therapies developed for each person has been shown to support autistic people in learning adaptive behaviors and coping strategies to deal with living in a world not designed for them, but treatment quality varies widely and there are ABA providers focused on contracts and monetary gain over the true benefit for the individual and their family, producing treatments that are less science-based, more harmful, and offer subpar benefits (Keenan et al., 2010). Kirkham (2017) points out that the modern neurodiversity movement claims ABA attempts to make autistic children act neurotypical, without concern for the mental health damage that repressing someone’s identity can have on a person. The same advocates claim autistic children do not require treatment just for being different from neurotypical people and ABA therapies should be carefully assessed before implementing on small children who are unable to defend themselves. Some posit that ABA done poorly trains children to be docile and do whatever adults demand, leading to autistic adults experiencing increased unwanted sexual experiences and sexual trauma as compared to neurotypical adults (Pecora et al., 2020). Research on adult autistic sexual experiences and ABA services received in childhood could answer this question more definitively. Evidence Based Treatment for Queer and Transgender Adults Transgender autistic people will often benefit from adapted treatment as communication and sensory challenges associated with autism and gender issues due to being transgender open the individual to discrimination and relational challenges on many fronts. According to Holt et al. (2021), 77% of transgender people seek therapy for gender identity issues and others seek therapy to manage internalized stigma, depression, anxiety, trauma, suicidal ideation, and substance use. It is often difficult for transgender people to find effective care as even providers from diverse sexually backgrounds may not understand diverse gender identities, and finding providers who accept and affirm the whole client and do not require the client to educate the provider on their gender identity is important (Snow et al., 2022). An important support for transgender youth is having parents and family that affirm and support their gender identity and provide them with access to gender-affirming treatment and family inclusion should not be neglected in treatment (Allen et al., 2021). Unfortunately, many of those who seek therapy will confront stigmatization from providers including misgendering and misunderstanding about gender in general that could be remedied by culturally responsive training for providers on transgender experiences and best practices in adapting treatment to meet transgender needs (Holt et al., 2021). Protective factors associated with transgender mental health are acceptance of self, self-esteem, being or having a role model, community and individual resources, and positive self-identity (Clements et al., 2021). Much like the autistic community, the transgender community also builds resiliency through technology such as social media posts, access to narratives and groups of other transgender people online, and intentional creation of a positive transgender self in a welcoming online environment before coming out in the brick and mortar world (Clements et al., 2021). Autistic LGBTQ+ people experience the double marginalization of being both autistic and queer and, as seen from previous research, autistic people are more likely to be bisexual. Wang and Feinstein (2022) found that bisexual individuals experience more mental health challenges, suicide risk, and substance abuse than either gay and lesbian and straight people but found protective factors that are worth exploring. They found that similarly to autistic resilience factors, support and acceptance from parents and peers, a sense of belonging, experiences with similar people, and positive self-identity development can reduce distress and internalized stigma and increase self-esteem and mental health. Embracing of bisexual identity is associated with increased mental health, resilience, positive associations with having unique perspectives, and ability to love without concern for sex or gender (Wang, & Feinstein 2022). Discussion for Section The neurodiversity movement is still relatively young and the idea that autistic people are simply different and not something to be corrected has not existed long enough for many solid research-based interventions to be evaluated on this premise. Evidence based treatments that have been found helpful for adult autistic queer people are practical lifestyle implementations of self-care, CBT, exercise, alternative treatments such as micro-dosing THC, LSD, or psylocibin, and therapy. Treatments that are controversial such as ABA should be given special attention before being implemented in a treatment plan. Although there is a wealth of research around families of autistic people and resilience, there is a lack of research on increasing resilience for autistic people themselves (Ghanouni & Quirke 2023) and what medications may reduce anxiety and depression for autistic people (Deb et al., 2021). More research needs to be done asking autistic people what they want to gain from treatment and what aspects of treatments they find most beneficial, much research is done in quantitative fashion and more qualitative information would be helpful in catering EBPs to autistic needs (Spain et al., 2020). Sample sizes for specialized research studies on autistic transgender individuals tend to be small and data collected is less reliable than larger sample sized would allow (Helverschou et al., 2019). Similarly, in research on alternative treatments using psychedelics, sample sizes from studies have been small, larger studies would need to be completed to know if possible side effect risks overwide the benefits from such treatments (Markopoulos et al., 2022). There may need to be different research into EBPs for people with and without intellectual disability and autism as effective treatments for these two autistic populations are likely to be different (Tse, 2020). While there is increasing research centered on transgender people, there are very few that look at non-binary populations by themselves and most transgender studies do not take into account sexuality among transgender people and how that may impact health (Holt et al., 2021). REFERENCES Allen, L. R., Dodd, C. G., & Moser, C. N. (2021). Gender-affirming psychological assessment with youth and families: A mixed-methods examination. Practice Innovations, 6(3), 159–170. https://doi.org/10.1037/pri0000148 Aran, A., Harel, M., Cassuto, H., Polyansky, L., Schnapp, A., Wattad, N., Shmueli, D., Golan, D., & Castellanos, F. X. (2021). Cannabinoid treatment for autism: a proof-of-concept randomized trial. Molecular autism, 12(1), 6. https://doi.org/10.1186/s13229-021-00420-2 Bemmer, E. R., Boulton, K. A., Thomas, E. E., Larke, B., Lah, S., Hickie, I. B., & Guastella, A. J. (2021). Modified CBT for social anxiety and social functioning in young adults with autism spectrum disorder. Molecular Autism, 12, 1-15. doi:http://dx.doi.org/10.1186/s13229-021-00418-w Clements, Z. A., Rostosky, S. S., McCurry, S., & Riggle, E. D. B. (2021). Piloting a brief intervention to increase positive identity and well-being in transgender and nonbinary individuals. Professional Psychology: Research and Practice, 52(4), 328–332. https://doi.org/10.1037/pro0000390 Deb, S., Roy, M., Lee, R., Majid, M., Limbu, B., Santambrogio, J., Roy, A., & Bertelli, M. O. (2021). Randomised controlled trials of antidepressant and anti-anxiety medications for people with autism spectrum disorder: systematic review and meta-analysis. BJPsych open, 7(6), e179. https://doi.org/10.1192/bjo.2021.1003 Djela, M. (2021), Change of autism narrative is required to improve employment of autistic people, Advances in Autism, 7(1), 86-100. https://doi.org/10.1108/AIA-11-2019-0041 Doherty, M., Neilson, S., O'Sullivan, J., Carravallah, L., Johnson, M., Cullen, W., & Shaw, S. C. K. (2022). Barriers to healthcare and self-reported adverse outcomes for autistic adults: A cross-sectional study. BMJ Open, 12(2) doi:https://doi-org.csu.idm.oclc.org/10.1136/bmjopen-2021-056904 Ghanouni, P., & Quirke, S. (2023). Resilience and Coping Strategies in Adults with Autism Spectrum Disorder. Journal of autism and developmental disorders, 53(1), 456–467. https://doi.org/10.1007/s10803-022-05436-y Hall, J. P., Katie, B., Streed, C. G., Jr, Boyd, B. A., & Kurth, N. K. (2020). Health disparities among sexual and gender minorities with autism spectrum disorder. Journal of Autism and Developmental Disorders, 50(8), 3071-3077. https://doi-org.csu.idm.oclc.org/10.1007/s10803-020-04399-2 Helverschou, S. B., Brunvold, A. R., & Arnevik, E. A. (2019). Treating Patients With Co-occurring Autism Spectrum Disorder and Substance Use Disorder: A Clinical Explorative Study. Substance abuse : research and treatment, 13, 1178221819843291. https://doi.org/10.1177/1178221819843291 Holt, N. R., Ralston, A. L., Hope, D. A., Mocarski, R., & Woodruff, N. (2021). A systematic review of recommendations for behavioral health services for transgender and gender diverse adults: The three-legged stool of evidence-based practice is unbalanced. Clinical Psychology: Science and Practice, 28(2), 186–201. https://doi-org.csu.idm.oclc.org/10.1037/cps0000006.supp (Supplemental) Hwang, Y. I., Foley, K.-R., & Trollor, J. N. (2020). Aging well on the Autism spectrum: An examination of the dominant model of successful aging. Journal of Autism & Developmental Disorders, 50(7), 2326–2335. https://doi-org.proxy1.calsouthern.edu/10.1007/s10803-018-3596-8 Keenan, M., Dillenburger, K., Moderato, P., & Röttgers, H.-R. (2010). Science for sale in a free market economy: But at what price? Aba and the treatment of autism in europe. Behavior & Social Issues, 19(1), Pages 126–143. Kirkham, P. (2017). ‘The line between intervention and abuse’ – autism and applied behaviour analysis. History of the Human Sciences, 30(2), 107–126. https://doi.org/10.1177/0952695117702571 Markopoulos, A., Inserra, A., De Gregorio, D., & Gobbi, G. (2022). Evaluating the Potential Use of Serotonergic Psychedelics in Autism Spectrum Disorder. Frontiers in pharmacology, 12, 749068. https://doi.org/10.3389/fphar.2021.749068 Mayor A. (2021). Exploring the views of young people with autism spectrum disorder (ASD) on how to improve medical consultations. BJPsych Open, 7(Suppl 1), S207. https://doi.org/10.1192/bjo.2021.553 Pecora, L. A., Hancock, G. I., Hooley, M., Demmer, D. H., Attwood, T., Mesibov, G. B., & Stokes, M. A. (2020). Gender identity, sexual orientation and adverse sexual experiences in autistic females. Molecular Autism, 11, 1-16. https://doi-org.csu.idm.oclc.org/10.1186/s13229-020-00363-0 Snow, A., Cerel, J., & Frey, L. (2022). A safe bet? Transgender and gender diverse experiences with inclusive therapists. The American journal of orthopsychiatry, 92(2), 154–158. https://doi.org/10.1037/ort0000599 Spain, D., Happé, F. How to Optimise Cognitive Behaviour Therapy (CBT) for People with Autism Spectrum Disorders (ASD): A Delphi Study. J Rat-Emo Cognitive-Behav Ther 38, 184–208 (2020). https://doi.org/10.1007/s10942-019-00335-1 Tse A. C. Y. (2020). Brief Report: Impact of a Physical Exercise Intervention on Emotion Regulation and Behavioral Functioning in Children with Autism Spectrum Disorder. Journal of autism and developmental disorders, 50(11), 4191–4198. https://doi.org/10.1007/s10803-020-04418-2 Wang, A. Y., & Feinstein, B. A. (2022). The perks of being bi+: Positive sexual orientation-related experiences among bisexual, pansexual, and queer male youth. Psychology of sexual orientation and gender diversity, 9(1), 58–70. https://doi.org/10.1037/sgd0000459
0 Comments
|
Details
Hello friends! I would like to publish writings from myself and other people with autism as snapshots of how autism has affected them, since there are so many misconceptions and confusions about adults with autism.
Some background: I completed a 12 unit certificate program to be able to serve autistic students and am angry at how the program focused only on little boys as autistic and completely left out adults, the trans autistic population, and girls/ femmes/ women autistics. I am currently pursuing a PsyD to do more research on autism and gender. Please contact me if you would like to add a story! If so, please send me your piece, publish name, title, and an image (can be a picture related to your content, your picture, an autism meme, etc). I am interested in publishing this collection, because people don't know enough about us (but sure do assume a lot). Also on Facebook! AuthorLisa Macafee, autistic counselor with a hankering for social justice. Archives
March 2024
Categories |
 RSS Feed
RSS Feed